Self Directed Rehabilitation
At present, upper and lower extremity (UE and LE) gains made in the clinic often do not generalize to actual use at home. Discrepancies between improvements achieved in clinic to daily use at home range from 33% in the affected arm to 100% for mobility and walking (Lang et al., 2023). There is a need to expand and develop innovative rehabilitation approaches that empower stroke survivors and their families to drive the recovery process and bridge the gap between the clinic and the home environment.
Self-directed training offers a solution to close this gap. Self-directed training is a structured rehabilitation program with clear patient objectives where therapeutic activities are completed independently by the patient in their real-world environment with clinician supervision outside of practice. In contrast to in-person therapy, adherence and engagement in unsupervised training is a major challenge because patients must practice on their own (Donoso Brown et al., 2015; Jurkewicz et al., 2011; Touillet et al., 2010).
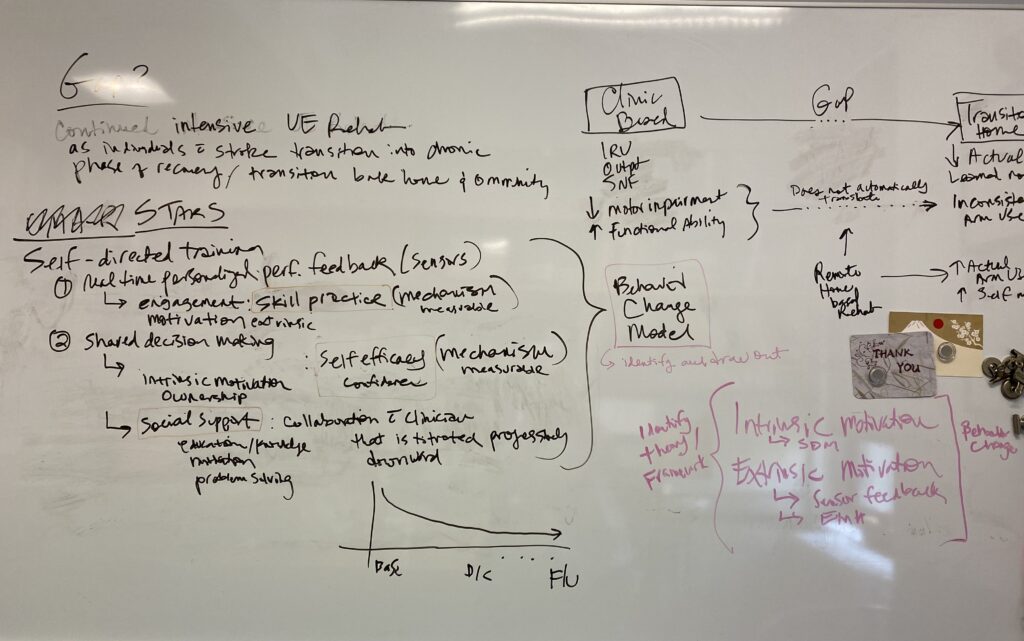
In order to develop effective self-directed interventions, PIVOT Lab is working on gaining a deeper understanding of the barriers and facilitators to self-directed training. One of our current projects is investigating the key component of self-directed training based on the perspectives of individuals with chronic stroke who completed a 4-week self-directed arm training program.
We recently completed a feasibility study for a self-directed arm intervention called the Use My Arm-Remote (UMA-R; Kim et al., 2024). UMA-R consisted of shared decision making, daily phone app, and weekly Zoom check-ins with an occupational therapist to increase real world use of the affected arm for individuals living at home in the chronic phase of recovery.
Key findings:
- Self-directed training was safe, feasible, and well accepted by participants. No drop outs, all participants that started the program finished. 100% would recommend UMA-R to other stroke survivors.
- Not only was the UMA-R safe and feasible to complete, participants also experienced improvement in satisfaction and performance of self-selected goals, real world arm use, and motor impairment.
References
References:
- Lang, C. E., Holleran, C. L., Strube, M. J., Ellis, T. D., Newman, C. A., Fahey, M., DeAngelis, T. R., Nordahl, T. J., Reisman, D. S., & Earhart, G. M. (2023). Improvement in the capacity for activity versus improvement in performance of activity in daily life during outpatient rehabilitation. Journal of Neurologic Physical Therapy, 47(1), 16-25. doi: 10.1097/NPT.0000000000000413. PMID: 35930404; PMCID: PMC9750113
- Kim, G.J., Gahlot, A.*, Magsombol, C., Capasso, N., Waskiewicz, M., Kim, H.*, Parnandi, A., Dickson, V.V., & Goverover Y. (2024). Feasibility of a self-directed arm training program for individuals living community after chronic stroke. Archives of Rehabilitation Research and Clinical Translation, 6(1), 100316. https://doi.org/10.1016/j.arrct.2023.100316
- Kim, G.J., Gahlot, A.*, Magsombol, C., Waskiewicz, M., Capasso, N., Van Lew, S., Goverover, Y., & Dickson, V.V. (2023). Protocol for a remote home-based upper extremity self-training program for community-dwelling individuals after stroke. Contemporary Clinical Trials Communication. 33, 101112 https://doi.org/10.1016/j.conctc.2023.101112
- Donoso Brown, E. V., Dudgeon, B. J., Gutman, K., Moritz, C. T., & McCoy, S. W. (2015). Understanding upper extremity home programs and the use of gaming technology for persons after stroke. Disabil Health J, 8(4), 507-513. https://doi.org/10.1016/j.dhjo.2015.03.007
- Jurkiewicz, M. T., Marzolini, S., & Oh, P. (2011). Adherence to a home-based exercise program for individuals after stroke. Top Stroke Rehabil, 18(3), 277-284. https://doi.org/10.1310/tsr1803-277
- Touillet, A., Guesdon, H., Bosser, G., Beis, J. M., & Paysant, J. (2010). Assessment of compliance with prescribed activity by hemiplegic stroke patients after an exercise programme and physical activity education. Ann Phys Rehabil Med, 53(4), 250-257, 257-265. https://doi.org/10.1016/j.rehab.2010.03.005
Shared Decision Making
Shared decision-making is a collaborative communication process where the patient and clinician make mutually agreed decisions based on patient values and priorities along with clinician expertise (Himmelfarb et al., 2023). Shared decision-making shifts the spotlight to the patient, requiring the patient to increase their autonomy and decision making to take a more active role in driving their recovery. The adoption of shared decision making in outpatient and home therapy settings can meet the shifting needs of stroke survivors as they relearn and adjust back to living in their home and in the community. We believe that patients in the chronic phases must start to drive their own therapy in order to successfully transition to their new home routines and community life.
The implementation of shared decision-making has been increasingly valued in healthcare because it improves quality of patient care in communication, equity, satisfaction, and adherence (Himmelfarb et al., 2023). The use of shared decision-making in rehabilitation has demonstrated greater improvement in UE function and motor abilities in acute stroke (Ikegami et al., 2023) and activities of daily living (ADL) in chronic geriatric community-based settings (Nagayama et al., 2016).
The results of our previous work reinforce the existing literature on challenges of implementing share decision-making from both the therapist and patient side. Clinician barriers for shared decision-making included perceived lack of experience in shared decision-making and need for patient buy-in, while patient barriers included lack of foundation knowledge in stroke rehabilitation (Gahlot et al., 2024). Clinician facilitators to implementing shared decision making included having competence with shared decision-making principles, and patient facilitators include trusting relationship with the clinician, and a personalized experience (Gahlot et al., 2024).
Current work on this topic includes the development of an implementation plan and strategies to facilitate clinical implementation of shared decision-making practices into stroke rehabilitation.
References:
- Gahlot, A.*, Richardson, G.*, Librea, P.*, & Kim, G.J. (2024). Clinician perspectives on shared decision-making with individuals with stroke during self-directed rehabilitation. Frontiers in Rehabilitation Sciences, 5:1414878, https://doi.org/10.3389/fresc.2024.1414878
- Himmelfarb, C. R. D., Beckie, T. M., Allen, L. A., Commodore-Mensah, Y., Davidson, P. M., Lin, G., Lutz, B., & Spatz, E. S. (2023). Shared Decision-Making and Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation, 148(11), 912-931. https://doi.org/doi:10.1161/CIR.0000000000001162
- Ikegami, M., Mutai, H., Karasawa, R., Yuzawa, Y., & Sakai, N. (2023). Effect of Upper Limb Function Training Combined with Goal Setting Using the Aid for Decision-Making in Occupation Choice for Hand Application in Patients with Acute Stroke. Asian Journal of Occupational Therapy, 19(1), 68-76.
- Nagayama, H., Tomori, K., Ohno, K., Takahashi, K., Ogahara, K., Sawada, T., Uezu, S., Nagatani, R., & Yamauchi, K. (2016). Effectiveness and cost-effectiveness of occupation-based occupational therapy using the aid for decision making in occupation choice (ADOC) for older residents: pilot cluster randomized controlled trial. PloS one, 11(3), e0150374.
Mobile Health Technology
Mobile health (mHealth) technology is defined by the World Health Organization as “medical and public health practice supported by mobile devices” (Malik et al., 2024). Includes the hardware devices like smartphones, tablets, activity trackers (e.g., fit bit), and wearable motion sensors. It also includes mobile health applications (mHealth apps), which are software programs used in smartphones and tablets to provide patients with a user interface to promote various health outcomes (Ramey et al., 2019).
- Smartphones, tablets—increasingly adopted and used by stroke survivors for communication (text, email, phone call), search for information, social media, calendar reminders, and games.
- Activity trackers, wearable sensors—which can collect motion data in real time in real world environments. Often used in conjunction with a mHealth app to monitor health behavior and provide performance feedback.
- mHealth apps – designed for use with smartphone and tablets to provide evidence-based information, support adherence to rehabilitation treatment plan, facilitate frequent communication between stroke survivors and clinicians, monitor health behaviors and rehabilitation progress
Ultimately, mhealth technology can improve rehabilitation services by delivering personalized interventions that extend the reach and access of rehabilitation services into real world environments (i.e., at home and in their community).
The PIVOT lab has explored stroke survivors’ attitudes and use patterns of smartphones (Kim & Kim et al., 2022), completed a scoping review of the application of wearables sensors for treatment and assessment in stroke rehabilitation (Kim et al., 2022), and used phone apps to promote daily communication with patients, and Zoom videoconference for weekly patient/therapist communication (Kim et al., 2024). In future studies, we will use wearable sensors to provide daily performance feedback of self-directed activities using a customized mHealth app.


